Healthcare Spending Gap
Introduction
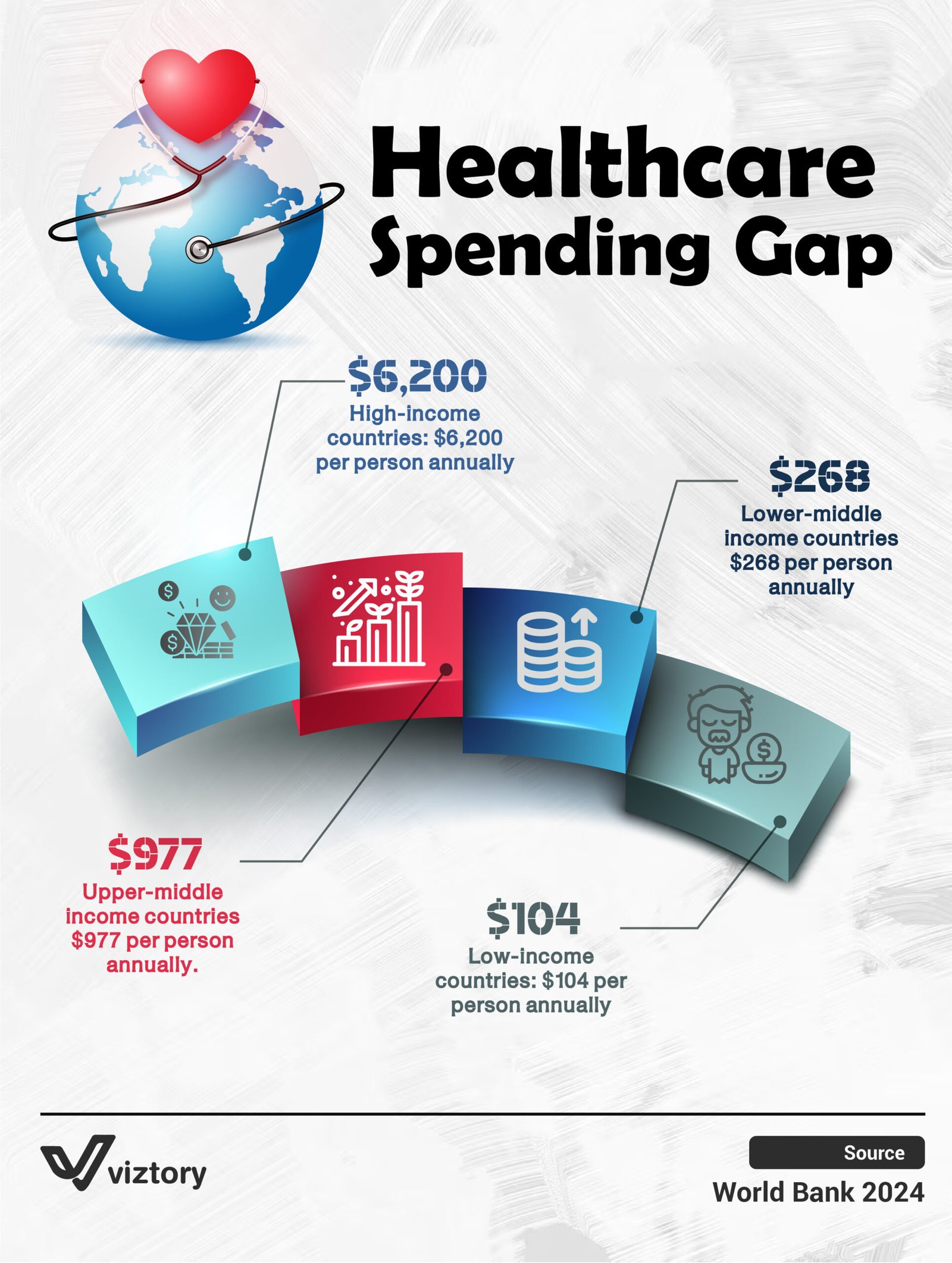
Healthcare inequality has become one of the most pressing global issues of our time. The infographic titled “Healthcare Spending Gap”, sourced from World Bank 2024, illustrates the vast differences in per capita health spending between countries of different income levels. From high-income nations investing thousands per person annually, to low-income countries struggling with under $110, this spending gap impacts everything from life expectancy to medical innovation.
Spending Highlights
According to the infographic:
-
High-income countries lead with an average of $6,200 per person annually, enabling strong healthcare systems, research institutions, and advanced medical infrastructure.
-
Upper-middle-income countries spend around $977 per person, showing progress but still far behind top-tier nations in healthcare access and quality.
-
Lower-middle-income countries allocate $268 annually per person, managing with limited budgets and often relying on international aid.
-
Low-income countries invest only $104 per person, which severely limits access to even the most basic healthcare services and facilities.
Why This Gap Matters
Healthcare is not merely a cost—it is a cornerstone of economic and social development. The spending gap influences several critical aspects:
-
Access to Care: Countries with lower spending often lack trained professionals, medications, and modern equipment.
-
Health Outcomes: Regions with minimal healthcare investment face higher rates of maternal deaths, infectious diseases, and preventable illnesses.
-
Medical Innovation: Wealthier nations have the advantage of investing in new technologies such as AI diagnostics, robotic surgery, and genetic treatments—technologies rarely accessible to lower-income nations.
Key Insights
Spending Does Not Equal Wasting
Higher spending, when managed effectively, correlates with better healthcare access, lower mortality rates, and improved quality of life.
Disparity Grows With Innovation
As technology becomes more central in healthcare, countries that cannot afford innovation fall further behind—not only financially, but medically and structurally.
Global Health Is Interconnected
Health crises originating in underfunded regions can escalate into global emergencies. The COVID-19 pandemic is a recent reminder that underinvestment anywhere poses a risk everywhere.
In-Depth Breakdown
The Economic Divide Is Growing
The difference in healthcare spending is not narrowing—it is expanding. As high-income countries invest in AI diagnostics, genomic research, and robotic surgeries, lower-income countries continue to struggle with basic healthcare delivery.
Richer countries are not just spending more; they are spending more efficiently, integrating digital records, predictive analytics, and personalized medicine.
Conversely, many low-income nations are still combating diseases like malaria, tuberculosis, and childhood malnutrition using minimal resources.
Efficiency Over Quantity
More spending does not automatically translate to better outcomes. Some middle-income countries have demonstrated that targeted investment—such as strengthening supply chains or expanding the role of community health workers—can deliver strong results with moderate budgets.
What Needs to Change
Key takeaways include:
-
Equity in Access: Global health strategies must shift focus from short-term relief to long-term infrastructure development and system sustainability.
-
Technology as a Bridge: Affordable digital tools like telemedicine and mobile health clinics can bring vital services to underserved communities at a fraction of the cost.
-
Local Empowerment: Training and empowering local healthcare professionals ensures sustainability and reduces dependency on foreign aid.
Conclusion
The healthcare spending gap is not simply a statistic—it reflects global priorities and imbalances. A child born in a low-income country is over ten times more likely to die from a preventable disease than a child born in a high-income country. This is not an accident; it is a consequence of systemic underinvestment.
To move toward global health equity, spending must not only increase—it must become smarter, more inclusive, and coordinated at the international level. In the interconnected world we live in, the health of each nation contributes to the health of all nations.