Ireland and Global Temperature Anomalies
-
Oct, Fri, 2024
Ireland and Global Temperature Anomalies: Implications for Healthcare
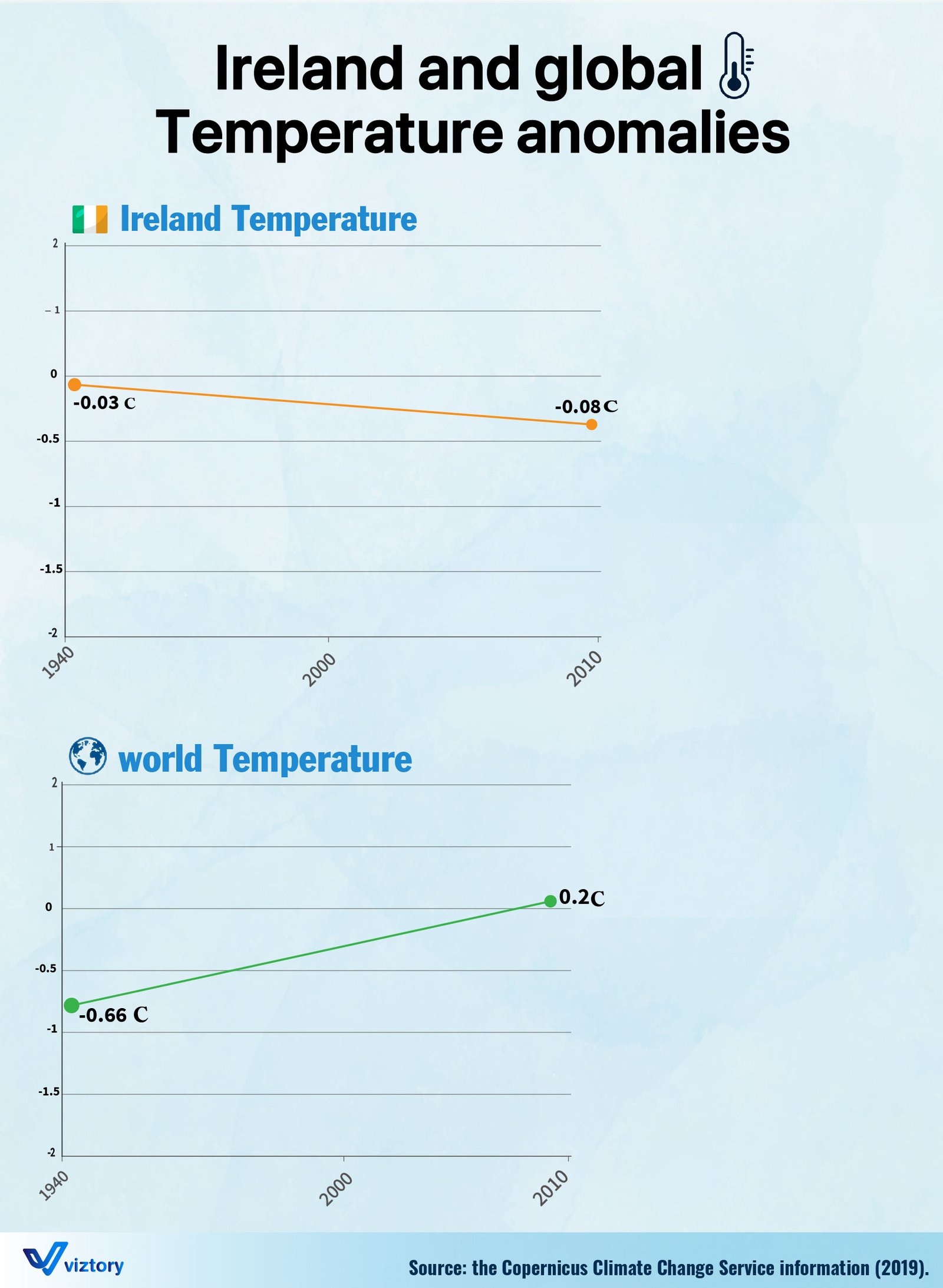
The visual representation of temperature anomalies for Ireland and the world over time indicates a clear disparity in regional and global climate changes. While Ireland’s temperature appears to have experienced a slight decrease from 1940 to 2010, global temperatures have shown a consistent upward trend. This discrepancy in temperature anomalies carries significant implications for healthcare systems, as climate change plays an increasingly important role in shaping health outcomes worldwide.
Climate Change and Public Health
Global temperature increases are linked to a broad spectrum of health-related challenges, from the spread of infectious diseases to the exacerbation of chronic conditions. As seen in the graph, the world experienced a significant rise in temperature, climbing from -0.66°C in the mid-20th century to +0.2°C in recent years. This global warming trend is a driving factor behind a wide range of health risks, including heat-related illnesses, cardiovascular stress, and respiratory issues.
For healthcare systems worldwide, these changes demand a reevaluation of healthcare strategies. Climate-related health risks require healthcare providers to not only address traditional diseases but also develop robust responses to emerging threats like heatwaves, vector-borne diseases, and air pollution.
Ireland’s Healthcare Response to Climate Variability
In contrast to the global trend, Ireland’s temperatures have shown a slight decline, from -0.03°C in the 1940s to -0.08°C by 2010. While Ireland may not be experiencing the same level of warming as other parts of the world, this variation still poses challenges. Colder temperatures can lead to increased mortality rates during winter months, as conditions like hypothermia and cardiovascular events become more common.
For Ireland’s healthcare system, the key is balancing responses to both colder and warmer seasons. Extreme weather patterns, whether they involve heat or cold, stress healthcare resources, requiring the system to be flexible and prepared to address a range of temperature-induced health concerns.
Global Climate Change and the Spread of Diseases
One of the most significant healthcare challenges posed by rising global temperatures is the increased spread of vector-borne diseases. As global temperatures rise, the habitats of disease vectors like mosquitoes and ticks expand, potentially introducing diseases such as malaria, dengue fever, and Lyme disease to new regions, including those that were previously unaffected.
For Ireland, the relatively stable temperature anomalies might seem to shield the country from some of these risks. However, globalization and increased mobility mean that Ireland’s healthcare system must also be prepared to manage imported cases of diseases that thrive in warmer climates. This requires a proactive approach to surveillance, early diagnosis, and public health education.
Chronic Diseases and Climate Change
Both cold and warm temperature extremes can exacerbate chronic diseases such as cardiovascular and respiratory conditions. In warmer climates, heatwaves put a strain on the cardiovascular system, increasing the likelihood of heart attacks and strokes. In colder climates, including Ireland, chronic respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD) are worsened by cold air, which can trigger exacerbations and hospitalizations.
The global rise in temperatures also exacerbates air pollution, which is a significant driver of respiratory diseases. Rising global temperatures, combined with industrial pollution, create conditions where air quality worsens, leading to higher rates of asthma and lung disease. Both Ireland and the rest of the world will need to focus on strengthening healthcare responses to air pollution-induced diseases.
Healthcare Adaptation to Climate Change
The global rise in temperatures depicted in the graph calls for significant adaptation in healthcare systems. For Ireland, despite the slight decrease in temperature anomalies, preparing for the wide-ranging effects of climate change on health is critical. The country will need to invest in improving healthcare infrastructure to deal with cold-related illnesses, while also staying vigilant about emerging global health risks associated with rising global temperatures.
For the world, climate change demands that healthcare systems build resilience and adaptability. Public health initiatives aimed at reducing exposure to temperature extremes, improving early warning systems for climate-induced diseases, and investing in climate-resilient healthcare infrastructure are crucial steps to protect population health.
Conclusion
The contrasting temperature anomalies between Ireland and the world emphasize the localized nature of climate change and its varied impacts on health. For both Ireland and global healthcare systems, addressing the health consequences of these anomalies will require targeted interventions. Whether it’s managing the health risks of colder temperatures in Ireland or adapting to rising global temperatures and their associated health challenges, healthcare systems must prioritize climate resilience to safeguard public health in an era of increasing environmental instability.